Authored by Michelle Mckeon
What is Lyme disease
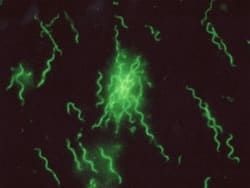
- There are 5 subspecies of Borrelia Burgdorferi, more than 100 strains in the US, and around 300 strains all around the world.
- Lyme disease is caused by a tick bite. However, fleas, mites, lice, mosquitoes, and biting flies can also transmit this disease.
- While it is thought that only deer carry this disease, birds, mammals, and rodents are also carriers.
Signs and Symptoms of Lyme Disease
- Lyme disease can affect multiple organs including the heart, skin, joints, and nervous system, producing a wide range of symptoms.
- Lyme disease has been called the great imitator and should be considered when diagnosed with rheumatologic and neurologic conditions, as well as Chronic Fatigue Syndrome, Fibromyalgia, ALS, MS, Parkinson’s, Dystonia and any other difficult-to-diagnose multi-system illness.
- There are three stages of Lyme. The first stage is known as Early Localized, the second stage is known as Early Disseminated, and the third stage is called Late Disseminated.
- Depending upon the stage, the symptoms can range from a rah, fatigue, headache, joint and muscle stiffness, and swollen glands, to Bell’s palsy, meningitis, confusion, neuropathy, arthritis, paralysis, tremors, and heart failure.
Lyme Disease Rash
- Fewer than 50% of patients with Lyme disease recall any rash.
- The rash that is most associated with Lyme disease is known as the erythema migrans (EM) or “bull’s-eye” rash. However, atypical forms of this rash are seen far more commonly.
- The rash can radiate from the site of the tick bite
- It is sometimes warm to the touch
- Appears about a week or two after transmission and persists for about three to five weeks
Where is Lyme disease
- Lyme disease is present in all 50 states and is most commonly found in the Northeastern part of the United States
- Ticks know no borders and respect no boundaries, as they are found throughout the world including Australia, Europe, Japan, and countries that were once a part of the Soviet Union.
- “I would therefore estimate that conservatively if 150-200 million people have Lyme disease in the world right now, then certainly at least one third of those could have been exposed to co-infections.” Dr. Richard Horowitz
- “We are in the middle of a rising epidemic of associated tick-borne co-infections, and we are not adequately monitoring the number of people affected. We are definitely underestimating the numbers!” Dr. Richard Horowitz
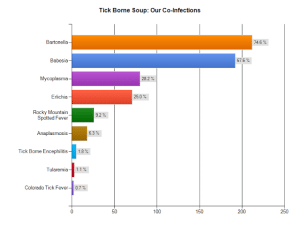
Co-infections
- Scientists have discovered more than a dozen tick-borne diseases in the United States and new ones are still being recognized.
- One tick may carry multiple pathogens and therefore the host can become infected with more than one co-infection from the bite of a single tick.
- Diagnosis and treatment can be more difficult for a patient infected with co-infections and/or secondary infections. Generally it results in a more severe illness, more symptoms, and a longer recovery.
- Some co-infections are Babesia, Bartonella, Anaplasma, Ehrilichia, Rocky Mountain Spotted Fever, Mycoplassma, Protozoa Rheumatica, and Powassan Virus. Though there are others both known and unknown.
- Secondary infections, such as viral infections, Candida, parasites, or C-Diff are often the result of severely compromised immune systems caused by the original infection.
Lyme disease treatment:
- There has never been a study indicating that 30 days of antibiotic treatment cures Chronic Lyme disease.
- There is an accumulation of documentation in the United States and throughout European medical literature demonstrating that short courses of antibiotic treatment are unsuccessful in eradicating Lyme disease.
- Through the return of symptoms most cases of chronic Lyme disease indicate an extended course of therapies to attain symptomatic relief.
Testing
- IGeneX in Palo Alto, California is one of the most reputable labs in detecting Lyme disease. Fry Labs in Scottsdale, Arizona is a state of the art lab for detecting co-infections.
- The Centers For Disease Control And Prevention (CDC) surveillance criteria for Lyme disease were developed to track a small band of cases for epidemiologic purposes. This surveillance criteria were never meant to be used as diagnostic criteria, nor were they meant to outline the complete scope of Lyme disease.
- By definition, a screening test should have at least 95% sensitivity. The Elisa screening test misses 35% of culture proven Lyme disease, making it only have 65% sensitivity.
- Of patients with acute culture-proven Lyme disease, 20–30% come out seronegative on serial western blot sampling. Antibody titers also seem to decline over time. Therefore it is not sensitive enough to identify the Lyme spirochete from a person with a chronic infection.